Introduction
In September 2000, the historical Millennium Summit gathered world leaders in New York to adopt the UN Millennium Declaration for the period 2000-2015, later to be called the Millennium Development Goals (MDGs) (UN Millennium Project 2000). Three out of the eight adopted MDGs concern improved health of the population, that is, reduced child mortality (MDG4), improved maternal health (MDG5), and actions to combat HIV/AIDS, malaria and other diseases such as tuberculosis. Of these goals, the one on maternal mortality and reproductive health has been the least successful while progress has been made in reaching MDG4 and MDG6, yet with much inter-country variability (United Nations 2015). The over-all experience of MDGs and its implementation paved the way for the Sustainable Development Goals (SDGs) 2016-2030, short-named Agenda 2030, adopted on September 25, 2015, during the General Assembly of the United Nations (Sustainable Development Knowledge Platform 2015). In contrast to the MDGs, only one out of 17 SDGs addresses health directly, that is SDG3: ‘Ensure healthy lives and promote wellbeing for all at all ages.’ This ambitious goal reminds of the slogan ‘Health for All by the Year 2000’ of the Alma Ata Declaration, adopted by the World Health Organization (WHO) in 1978 (World Health Organization 1978). It was widely felt that the declaration aimed to address the healthcare needs in low-income countries (Gillam 2008), but it has nevertheless also influenced implementation of primary healthcare (PHC) in industrialized countries, including Iceland.
In short, PHC as spelled out in the Alma Ata Declaration (World Health Organization 1978; World Health Organization 2008) can be described as being composed of three main dimensions of health care services. The first one relates to the eight principal elements of healthcare delivery: access to essential medicines; treatment; preventive services; immunizations; focus on services for mothers and children, including family planning; food and nutrition; and access to water and sanitation. In addition to these eight key elements of Alma Ata, there is emphasis on proper lines of referral, that is, to have people seek care at the most appropriate level of the healthcare system, be it in the community, in a health centre (1. level), hospital (2. level), or in more advanced and specialized health care units or hospitals (3. level). Thus, community participation all through the healthcare system is one additional dimension to a well-functioning PHC system. The two above dimensions are nevertheless not enough to satisfy the need of the population for healthcare services. The services need to be ‘accessible,’ ‘available,’ ‘appropriate,’ and ‘affordable’ (the 4As). This adds the third dimension to the PHC model and addresses the inner functioning of the healthcare system. This dimension includes administration and management, human resources, physical infrastructures, research, and collection of health information data. All three dimensions of the PHC system as envisioned in Alma Ata need to fit properly with each other to perform efficiently and effectively. Despite controversies regarding the success of the implementation of Alma Ata for primary healthcare with genuine community participation, today it is still as relevant as it was in 1978 (World Health Organization 2008; Lawn et al. 2008).
The Icelandic International Development Agency (Iceida) supported the health services in the Monkey Bay area in Mangochi district in Malawi in southern Africa in the period 2000-2011. The aim of this paper is to describe and analyse the activities of the Monkey Bay Health Care Project (MBHCP) through the lens of several monitoring and evaluation methods. In particular, focus will be given to different process indicators used during the collaboration while some consideration is also given to structural and outcome indicators. The results are then discussed and lessons learned summarized.
Evaluation and monitoring of health projects
Evaluators of development projects and assistance are faced with increasingly complex situations (Conlin and Stirrat 2008; Segone 2008). These trends are mainly related to the current architecture of aid following the Paris Declaration on Aid Effectiveness in 2005 with the concepts alignment and harmonization becoming central. One important tendency is to evaluate large themes while less importance is given to projects and programs evaluations. The focus is on strategies and resource allocation and the importance of measurable impact is underlined. Likewise, consequences of development assistance for social equity are to be considered as well as enhancement of empowerment. The evaluation procedures are thus more complex and the contribution of particular donors has become increasingly fluid, for example assistance with funds through sector wide approach (SWAp). Another important recent trend in evaluation has to do with focus on the MDGs and corresponding indicators (Conlin and Stirrat 2008). MGDs include also a move away from project-orientated interventions to a wider approach where other factors than the intervention alone should be taken into consideration.
There are several approaches available to monitor healthcare and delivery of services. The most common one is to make use of daily registration routines that are found all over the healthcare system. In low-income countries, including those in sub-Saharan Africa, most registration systems are based on paper records. This paper-based collection of data often includes information such as the name, sex, age and address of the attendee, and often diagnosis and treatment. This information is then transferred manually to daily, weekly or monthly summary sheets that are sent to the next level of the healthcare system for compilation across the respective health area/sector/district and then to national health authorities for trimestral, bi-annual or annual reports. Increasingly the higher-level analysis is done with the help of computers where data from the health centres is manually entered in appropriate computer programs. The quality of the data is however often of uncertain value (Gerrets 2015), and often no feedback is given to those who actually produce the data, that is, the frontline health workers in the healthcare facilities. The outcome is that the data collection lacks focus and over-burdened staff pay less than desirable attention to details and quality of the information provided. Actually, similar problems are found with data collection in high-income countries.
Another monitoring approach of healthcare services is conducting different types of surveys in the population being served. As there is no existing central population registry available in low-income settings, several approaches have been developed. Commonly known surveys are the ‘Demographic Health Survey’ (DHS) (The DHS Program 2015) to monitor health and population trends and the ‘Multiple Indicator Cluster Survey’ (MICS) on the health and wellbeing of children and women (Unicef 2015). In such surveys the household with its ‘head’ is the point of departure despite its complexities as a social unit for people where they live (Kriel et al. 2014; Randall, Coast, and Leone 2011). Another well-established method is the cluster sample technique initially developed to monitor vaccination coverage, but has also been applied to address other healthcare issues of interest for healthcare services and policy makers (Bennett et al. 1991).
Qualitative approaches are also of importance to gather information on the healthcare services from the viewpoint of providers as well as users. Despite the methodology does not allow great number of participants, it can give valuable insights in the functioning of the healthcare services, as well as the healthcare needs of the population. Further, mixed methods are also used, that is both quantitative and qualitative methods (Bamberger 2012)
Project evaluators often face considerable challenges to address all the complexities in a project setting. ‘Shoestring evaluation’ approach aims to offer evaluators tools that guarantee an evaluation with maximum quality possible, despite being conducted within a small budget, short time and with limited access to data (Bamberger et al. 2004). The approach is based on group discussions with the most important stakeholders, appraisal of strategic documents, interviews with the managers, and assessment of the decision-making processes. It focuses on inputs, implementation, outputs, and impacts, in addition to project design and factors that may influence implementation and outcome. This includes examination of the economic, political and organizational context and the socio-economic character of the population with emphasis on identification of eventual excluded groups.
Indicators have increasingly been used for global governance, including public and global organizations, non-governmental organizations (NGOs), or the private sector (Davis, Kingsbury, and Merry 2010). Examples abound, including the MDGs and SDGs (UN Millennium Project 2000a; ICSU and ISSC 2015). Well-constructed and relevant indicators have also the potential to quickly give knowledge on performance of activities in different sectors of society. A good indicator is a specific, observable and measurable characteristic that can be used to show changes or progress a program is making toward achieving a specific outcome.
Indicators are an important feature of all evaluation efforts. Indicators help us understand a system, compare it and improve it. There are several definitions of indicators, such as: (1) A quantitative or qualitative factor or variable that provides a simple and reliable means to measure achievement, to reflect changes connected to an intervention, or to help assess the performance of a development actor” (OECD/DAC 2010); or (2) A variable, which purpose it is to measure change in a phenomena or process (Kumar 1989). The European Commission describes (planning) indicators as: a description of the project’s objectives in terms of quantity, quality, target group(s), time and place (MDF Training and Consultancies 2005).
To inform the general public and funding bodies on their achievements, development agencies desire whenever possible to present concrete results through the use of diverse set of indicators. The acronym SMART is used to describe desirable characteristics of indicators, that is they should be Specific, Measurable, Achievable (acceptable, applicable, appropriate, attainable or agreed upon), Relevant and Time-bound (Better Evaluation 2015). On the other hand, the acronym SPICED relates more to how indicators should be used. They are Subjective (informants have a special position or experience that gives them unique insights), Participatory (involve the project’s ultimate beneficiaries, local staff and other stakeholders), Interpreted and communicable (may need explanation as they are locally defined), Cross-checked and compared (the validity of assessment needs to be cross-checked, by comparing different indicators and progress, and by using different informants, methods and researchers), Empowering (allow groups and individuals to reflect critically on the changing situation) and Diverse and disaggregated (indicators from a range of groups, especially men and women).
Whatever the indicators used, being SMART, SPICED or any other combination, for evaluation of health care services they can conveniently be grouped into three broad categories (Donabedian 1988). ‘Structural indicators’ describe the context of health care services, including physical structures, staff, equipment, and financing, and are usually the most easily obtainable indicators to monitor within a health project. ‘Process indicators’ are more difficult to obtain but measure activities that are supposed to lead to the desired outcome of project activities. They measure the interaction of patients with the healthcare delivery system. They are called proxy or indirect indicators when they refer in an indirect way to the desired outcome (MDF Training and Consultancies 2005). The indicator “proportion of children fully vaccinated by the age of 12 months” is, e.g., a process indicator if the over-all objective is to lower infant mortality rate (IMR), and vaccination at young age is an evidence-based mean towards that end. ‘Outcome indicators’ refer to the effects of the healthcare services on health status of patients and populations, for example mortality and morbidity rates. They are also called ‘direct indicators’ as they refer directly to the subject they were developed for (MDF Training and Consultancies 2005).
Global partnership for development and Iceida
Most low-income countries, particularly those in sub-Saharan Africa, are characterized by underfunded health sector. Common problems include lack of or deficient maintenance of physical infra-structure, lack in human resources that are adequately trained, communities that are difficult to reach, sporadic ambulance services, uncertain delivery of medicines and medical supplies, lack of appropriate laboratory services, and other key components of a well-functioning health care services. Thus, the MDG8 addresses the need for countries to develop a global partnership for development (UN Millennium Project 2000). In the case of Iceland, this has partly been achieved through the work of the ‘Icelandic International Development Agency’ (Iceida), currently active in three partner countries, that is Uganda, Mozambique, and Malawi (Iceida n.d.).
Iceida became involved in development assistance with Malawi through its support to the Bunda College of Agriculture (1993-2009), and its support to construct primary schools in Mangochi District (1995-2009). In the year 2000, Iceida expanded its activities in the country when it embarked on its most ambitious development project within the healthcare sector in the Monkey Bay area, one of five health areas in Mangochi District in southern Malawi. Later, in the period 2006-2010, assistance was given to the national adult literacy program, to improve water-and-sanitation in the area, and small-scale offshore fisheries technology in the villages by the Lake Malawi. At termination of the activities in Monkey Bay in the end of 2011, and based on achieved experience and results, in 2012 the Agency expanded its development support to involve all of the Mangochi District Council to improve basic services in the district (Iceida 2012).
In the period 2000-2011, the Government of Iceland through Iceida and the Government of Malawi (GoM) through the Ministry of Health (MoH), collaborated within the health sector in the Monkey Bay health zone area, one of five zones within the District of Mangochi in the South Region of Malawi. The agreement was based on a Project Document, elaborated following a feasibility study for the collaboration, conducted in October 1999 by one of the authors (GG). During the first four years of project implementation (2000-2003) the main emphasis of activities was on the improvement of physical structures of the health centre in Monkey Bay, the embryo to later become Monkey Bay Community Hospital (MBCH), as well as health zone area logistics and communication.
The second part of the collaboration (2004-2008) built on gained experience and aimed to consolidate what had been achieved in the first four years. Special emphasis was on the quality of the health services in MBCH and the health centres in the area, outreach activities, and training of Traditional Birth Attendants (TBAs), Community Based Distribution Agents (CBDAs) and Health Surveillance Assistants (HSAs). Training of human resources was a key activity and included up-grading and short courses and seminars for several categories of staff. Further, physical structures were expanded for the governmental run services in Monkey Bay and Nankumba, including staff houses.
In the third and last part of the collaboration (2009-2011), infrastructures were expanded in Monkey Bay, including a new and spacious maternity ward and laundry. Further, the out-patient (OPD) and the under-five (U5) clinic were expanded and renovated. In addition, four more staff houses were built in Monkey Bay. During this last phase of project activities, the health dispensary in Chilonga was transformed to become the third governmental health centre in the area with the construction of a new maternity wing. Further, three staff houses in Chilonga were renovated and two new constructed with contribution from community members.
During the three phases of the collaboration, ICEIDA gave logistical support through ambulance services and motorcycles (MCs) for out-reach activities. Internal administration and management has also been supported as needed, as well as radio communication between the health centres and MBCH. Further, along the years upgrading of staff was given a high priority, including both in- and out-of-country training. ICEIDA has basically been supporting governmental structures within the Monkey Bay area. At the same time, along the years of ICEIDA involvement in the area, it has facilitated the inclusion of health service providers in the area that are organized within Christian Health Association of Malawi (CHAM). This has, e.g., included participation in health zone meetings including discussion on the performance of the health care services, as seen in the HMIS, local training, MCs, and radio communication.
Along the years, the following five main objectives guided the project implementation:
1 Improve and upgrade infrastructure and equipment of the MBCH to progress towards standards defined by the GoM for community hospitals in order to operate as first line referral for health centres within the zone.
2 Increase operational capacity of community health related services in the zone with logistical support, training and infrastructure.
3 Operational community health related services
4 Functional health management information system
5 Collaboration between stakeholders within the health sector in the Monkey Bay health zone, in particular Mangochi District Health Management Team
Setting and methodology
The data presented in this paper is based on published and unpublished documents on the MBHCP. Data of the performance of the healthcare services is taken from the national Health Information Monitoring System (HMIS) in place in Malawi since 2002, including Monkey Bay (Ministry of Health 2009). It is enriched with data from research assignments and published results of Icelandic and Malawian university students and both authors (GG, JE) who applied diverse research methodologies in their research, including quantitative and qualitative approaches.
Malawi is situated in the heart of south-eastern Africa. It is landlocked and shares borders with Tanzania, Mozambique and Zambia. Out of a total area of 118.486 km2, Lake Malawi accounts for a fifth. During project implementation Malawi had a rapidly increasing population, with a population of about 14 million people (2011) that gives a population density of about 159 persons per km2 (Lake Malawi excluded). (Figure 1)
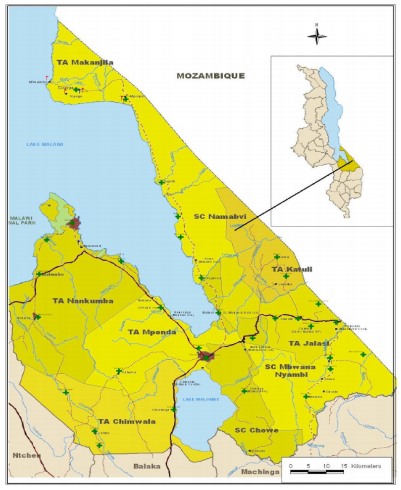
Malawi is divided into three administrative regions: the North, Central and South. The regions are further divided into 27 districts (six in the north, nine in the centre and 12 in the south). Following decentralisation that was initiated by the GoM in 1998, district authorities through District Assemblies, were delegated more power of administration and decision in matters that related to the governmental services, including that of health care delivery. In addition, districts are divided into Traditional Authorities (TA) that are made up of a group of villages. The villages are the smallest administrative units headed by a Village Headman/Headwoman. A group of 5-7 of these are clustered into one larger village unit, headed by a Group Village Headman.
The District of Mangochi is in the Southern region with population estimated to be about 827.756 (2009/2010 data). The district is divided into five health areas, of which Monkey Bay is one. MBCH is a governmental health facility and has the primary responsibility for all health related activity in area with about 100 villages and about 138.000 inhabitants (Table 1).
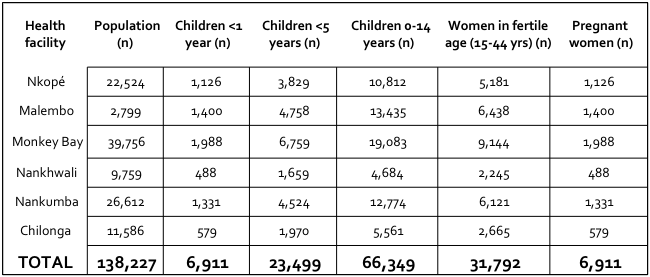
The government also runs the Nankumba health centre as well as the dispensary in the nearby Chilonga village. The dispensary was however dysfunctional for some years until it was up-graded in 2011 to become a proper health centre. In addition to the governmental services that are free of charge, there are four privately run health facilities in the area that apply user-charges. Three facilities are part of CHAM, i.e. Nkopé, Malembo and Nankhwali, and one is an Irish NGO, Billy Riordan Memorial Trust Clinic in Cape Maclear.
Results
Stuctural indicators
Physical infrastructures. In short, physical infrastructures were expanded and improved during project implementation. However, the objective to have MBCH to become a fully-fledged community hospital, in line with national standards, was not reached. For MBCH to become one it lacked a special paediatric and isolation wards, kitchen, X-ray department and a Nutritional Rehabilitation Unit.
Financial aspects. In the period 1999-2011, the total costs for project implementation on behalf of Iceida are estimated to be just less than $7.5m. The most costly component was the construction and renovation of governmental infrastructures in Monkey Bay, Nankumba and Chilonga. In real terms, the investment during 13 years has been about 54 US$ per capita living in the Monkey Bay area or about 4 US$ per capita and year. Evaluation of total costs needs to take into consideration the deplorable situation of the health services in the area at the start of project activities.
In the year 2010, over half of the funds (52%) were for so-called non-currents assets (vehicle maintenance, equipment hire and purchase, and equipment maintenance); operational costs (26%) included fuel and lubricants, rentals/accommodation and telephone/airtime; administrative costs (20%) were divided on stationery, guard services, meetings (refreshments), newspapers and allowances; and other costs (2%) were reimbursement, bank charges and miscellaneous.
Logistics. At the start of project activities in the year 2000, there was no ambulance in Monkey Bay. However, there was one in Nankumba health centre but difficulties to run it and fund recurrent costs. During project implementation ambulance services with cars purchased by Iceida with government drivers have been a key to reach out to the population in the rural villages. Until recently, two ambulances bought and run by ICEIDA funds have been stationed in MBCH with two drivers who are governmental employees. In addition to the ambulances, one utility vehicle has been bought to service MBCH to alleviate some of the minor tasks of transport off the ambulances.
In the year 2000, there were three MCs earmarked for services of two vertical programmes in the area, i.e., the bilharzia control programme and Save the Children Fund. MCs are however crucial for the health services in the area, especially for out-reach activities. ICEIDA has funded nine MCs in the Monkey Bay area (Nankumba, Chilonga, Malembo, Nankwhali, Nkopé and four at MBCH, i.e., for the Assistant Environmental Health Officer (AEHO), clinical coordinator, cold chain technician and the PC). All have been functional.
Staff. All health professionals who delivered services were Malawians on government payroll. As a general rule, Iceida applied a policy of no topping-up of salaries. Yet, one Malawian health professional was recruited in 2004 and was paid by the government but Iceida topped-up his monthly salary for his function as a national coordinator of project activities. Further, for a short period of time 2-3 other Malawian health professionals with key functions within the services had monthly extra salary, paid by Iceida. To learn and acquaint itself with the reality in the field, Iceida recruited Icelandic technical assistants (nurses, midwives, and medical doctors) who were placed in Monkey Bay in the period 2000-2008, one or two at a time. Further, one of the authors (GG) was a permanent consultant for Iceida that included more or less annual field visits in the period 2002-2011.
Process indicators
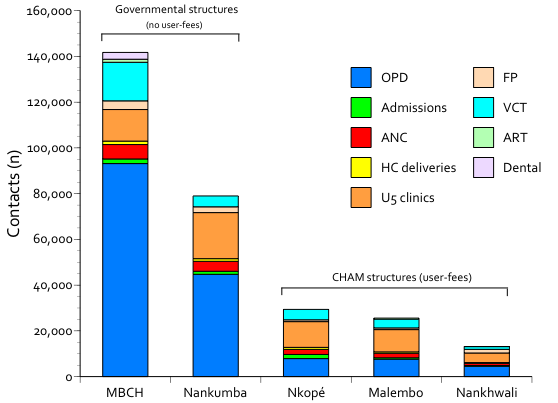
Out-patient activities (OPD). At the project start, the officially registered number of attendees to Monkey Bay health centre was high, considering the low number of staff and deficient quality of the physical facilities. At the time of the inauguration of the new hospital building in June 2002, the worn down health facility functioned more as a simple health centre (including skilled birth assistance) than a proper hospital. Nevertheless, the health information data indicated high number of attendees; in the period 2000-2002, the average registered number of attendees per month was 27.570 (median 20.956, range 10.640-62.656). At closer scrutiny, these numbers were inflated. In the period 2003-2011, after corrective measures had been taken to improve data collection, comparable registered number of attendees was 5.199 (median 4.842, range 2.232-10.702). Still in 2004, a study conducted by a Malawian medical student concluded that the HMIS was not functioning optimally to provide timely, valid, and accurate information (Salimu 2004). Improvement in data collection was thus continuously in focus during project implementation. Based on improved monitoring and cross-checking of data through multiple sources, the development of the number of attendees to OPDs in the five health facilities in the area give a reasonable indication of the development of the health services along the years of project implementation. (Figure 2).

In the OPD registration book, the age of the attendees is written down. Yet, in the HMIS age-groups of children are clumped together. To look further into the age-structure of attendees, one Icelandic medical student was given the task to go through the registration books in March 2005, and register the age of attendees in addition to registered diagnosis of children less than 5 years (Ragnarsson et al. 2006). In the two governmental health facilities, about 3/5 of the attendees were adults, compared to about 2/5 in the CHAM facilities. Taking into account the estimated number of children in each health centre catchment area, it was 1.22 more likely (RR 95% CI 1.18-1.16) that children 0-4 years old were taken to a CHAM facility compared to older children (RR 1.46, 95% CI 1.42-1.51), while adults were 1.16 (RR 95% CI 1.12-1.19) more likely to attend health facilities run by the government. Further, across the five health facilities, on average 57% of the attendees were females (range 47-63); such a difference was not noted among children.
To evaluate clinical quality of the services, the application of IMCI (Integrated Management of Childhood Illness) was studied (Ragnarsson et al. 2006). Eight out of 10 health professionals who attended sick children had been trained in applying IMCI. About 4/5 of all diagnosed disease groups were part of IMCI, with half being malaria, 28% respiratory infections, 6% with pneumonia, 5% with diarrhoea and the rest with diverse ailments.
Data from the HMIS indicate that government structures bear the main burden of delivering health services to the population in the area. In the year 2010, staff at MBCH had about 140.000 contacts and those at Nankumba about 80.000 contacts These contacts include services to those who are sick as well as preventive activities, both in the health facility and in the communities through out-reach activities. (Figure 3).
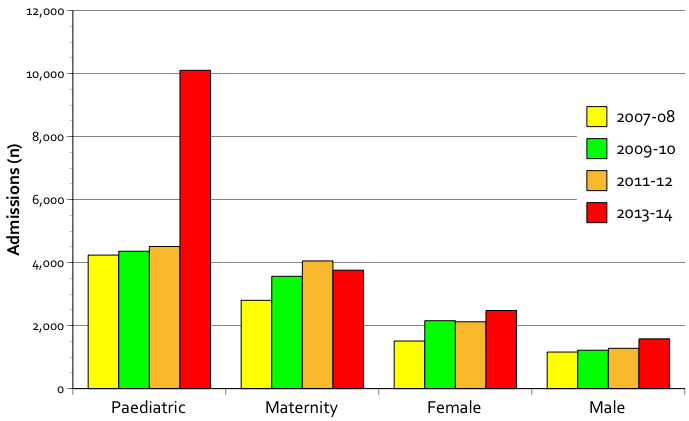
Admissions to MBCH. During project implementation the bed capacity of MBCH increased from a few beds to total 105 beds: maternity ward (n=34, can be expanded to 48), labour beds (n=8), nursery (n=7), paediatric ward (n=30), male ward (n=11), and female (n=15). The expansion of ward beds was taken cautiously after experience of few admissions after inauguration of the hospital in 2002; yet after 2004 the hospital wards have at times been over-full, and still more wards and beds are actually needed.
In the period 2006-2014, in total 54.851 patients were admitted to the wards of MBCH out of the total number of admissions, 24.772 (45%) were children, 15.382 (28%) in the maternity, 8.945 (16%) the female ward, and 5.752 (11%) in the male ward. On average there were 17 admissions per day. (Figure 4).
Antenatal care (ANC). Data in the HIMS indicate little changes in ANC attendance in 2002-2010 with on average 2.85 (range 2.46-3.08) visits during each pregnancy. National guidelines recommend pregnant women to attend their 1st ANC during the 1st trimester; in 2007 on average 4.3% (range 1.7-8.9) of pregnant women complied to that recommendation in the different healthcare catchment areas, and there is no indication that this has later improved.
In 2003, by applying cluster-sample technique, 215 randomly selected mothers were inquired about their ANC card for their last pregnancy (or history, if card was not available) (Fjalldal 2004). All except four had attended ANC at least once, and the average number of visits was 4.1 during the pregnancy. The first visit was on average at 24 weeks of gestation. In general the mothers expressed satisfaction with the services, and felt it was important to attend, in particular to have physical examination, and see that all was well with the growing foetus.
Deliveries. One of the targets of MDG5 was to have at least 75% of deliveries attended by skilled birth attendants. The first requisite to achieve that number is to have pregnant women to attend the ANC services; this has not been a problem in Monkey Bay health area (Fjalldal 2004). The second is to offer services that are attractive to them and where they feel secure to deliver, preferably with their mothers. Constraints to reach the MDG target include but are not restricted to deficient facilities without the option for surgery in case of need, less than optimally trained staff, and lack of ambulance services, often during the night.
During the project implementation, work with community members was given a high priority, in particular training of TBAs. At the peak of such activity, in 2006, there were about 140 TBAs working in the area. Twenty of them were newly trained and all the other had been on refresher courses. In addition to TBAs, there were registered 167 CBDAs who were either newly trained (n=20) or had attended refresher courses, and this activity reached deep into the communities in the health area (Gunnlaugsson and Einarsdóttir 2009).
In qualitative interviews with TBAs, it was found out that they were in general older women who had had children themselves and had learned the trade from family members (Stefánsdóttir 2006). They were respected in the community, considered to possess important life-skills for its members. One of every three TBAs had her own birth shelter and those without one attended births at the home of the delivering woman; this was considered an important constraint in their work. They appreciated their training but felt lack of proper supervision. In their opinion, the most useful things for the job were gloves (initially not distributed to the TBAs as a national policy), umbilical thread, cotton and anti-infective, lamp and tray, all provided by the project.
Abruptly, in October 2008, the Government of Malawi banned all deliveries by TBAs, to their and the mothers despair (Gunnlaugsson and Einarsdóttir 2009). The village headman was to enforce the law, and fine women who defied the rule and delivered with the help of a TBA, or had no other choice. Such a change of policy was intended to result in increased number of deliveries with skilled birth attendants, as aimed for in MDG5. This is also borne out by analysis of the HMIS data. These indicate a surge in numbers of women delivering in all the health institutions in the Monkey Bay area following the ban (Figure 5).
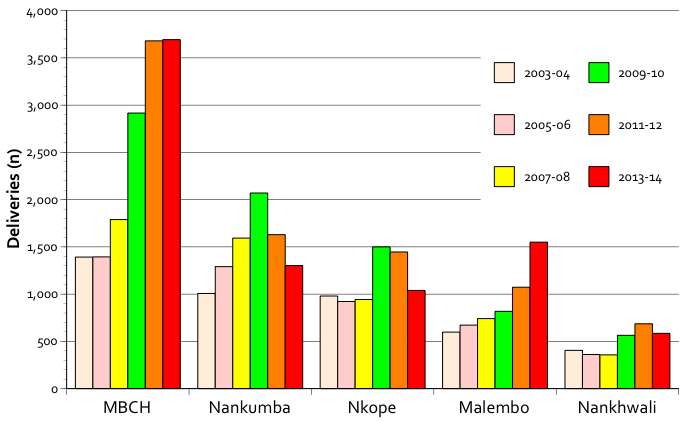
Yet, despite improved government facilities for delivery, comparison of the number of women delivering in MBCH compared to the number of those who attend ANC services for the first time show that about 1/4 of expected deliveries are still unaccounted for. Similar situation can be observed in the other health facilities. Some may deliver in Mangochi District Hospital, but without doubt there are still many who deliver at home, presumably assisted by a local TBA.
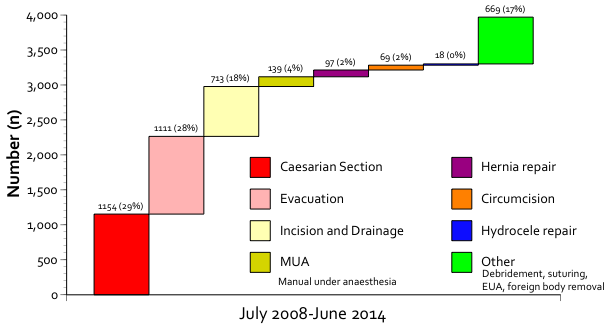
An important ingredient in delivery services is access to surgery, for example in case of obstructed labour. Since July 2008 there has been a functional surgical theatre operating in MBCH. At the end of June 2014, 1154 (29%) surgical operations were Caesareans out of a total of 3970 operations or on average 16 sections each month (Figure 6).
To analyse obstetrical practices in MHCH, one study was conducted to analyse in detail all deliveries in the hospital during one month in 2005 (Eythórsson, 2005). In total 87 women came to deliver but 19 were referred to MDH because of an impending Caesarian section. Out of the 68 deliveries in MBCH, one had been referred to MBCH from other health facilities in the area. The outcome of four pregnancies was still-birth, including two with breech presentation.
Newborn care. To analyse the care of newborns in MBCH, one study was conducted in the neonatal ward of the hospital (Guðmundsdóttir 2006). During March 2006, 34 newborns were admitted, thereof 22 within the first week from birth. Most were suspected to have sepsis (74%), and about one in five with birth weight <2500 g. It was concluded that administration of the two most important drugs (gentamicin and benzylpenicillin) was not according to guidelines with most of the newborns given too high (or too low) doses. Further, nursery routines were found to be deficient, for example regarding weighing and registration in clinical records.
Immunization coverage. Immunization is one of the important components to improve child survival. To have baseline data on the coverage, a study was conducted in 2003 on a random sample of 217 children who were selected through cluster-sample technique (Bennett et al. 1991; Þórðarson et al. 2005). The result shows that the coverage of BCG for children 12-23 months of age was 97% and most vaccinated with three doses for DTP and polio, indicating good access. There was however a trend for dropout of children in the vaccination programme with increasing age; 78% were vaccinated for measles and 70% of the children were fully vaccinate.
One indicator in the HMIS is the proportion of fully vaccinated children by the age of 1 year, as recommended by national guidelines. In the year 2002 data indicate that 35% were fully immunized compared to 58% in the year 2010; for the period 2002 to 2010, on average 52% (median 53, range 35-69) of the children were fully vaccinated by one year of age. Based on this result and comparing with the above cited immunization study there are reasons to believe that vaccination coverage in the area has increased during project implementation. Further, clinical experience, supported by HMIS data on reported cases of measles, give reasons to believe that measles was not epidemic in the area in the project period, indicating good vaccine coverage.
Out-reach clinics. Preventive health services to mothers and children are delivered both through clinics in the health facilities (static clinics) and through out-reach in the rural communities. At times during outreach, both maternal-and-child health services are to be given concurrently, but for several reasons that is not always the case. The out-reach clinics are often held in open-air spaces with no room for privacy, and in some places with little shelter for rain or sunshine. In the period 2006-2014 there were on average each year 52.471 children under 5-years of age who attended out-reach clinics in the Monkey Bay area (median 53.637, range 39.159-62.264). About 3/5 of the just less than half a million children who attended the clinics in the period were seen by a public service health professional.
In a quantitative study the implementation of out-reach clinics in the MBCH health area was investigated in the period January 2005 to March 2006 (Jónsdóttir 2006). Out of planned 480 sessions, 335 (74%) were conducted in the period. Positive findings were that there was a good calendar for out-reach clinics that offer a range of evidence-based services, for example vaccination, growth monitoring and distribution of vitamin A. Yet, the implementation was irregular, at times shortage of vaccines and vitamin A, monitoring of growth routines left room for improvement, and storage and quality of registers inadequate. Other structural problems identified to execute outreach clinics according to plan was heavy rain, bad roads, lack of transport, and lack of staff.
Prevention of malaria. Malaria was in a study found to be about half of all diagnosis of children less than 5 years (Ragnarsson et al. 2006). In a quantitative and qualitative study on malaria and its prevention in the Monkey Bay health area, it was concluded that 32-46% of about 200.000 attendees were given a malaria diagnosis in the five health facilities, most during the rainy season (Snæbjörnsson 2007). Yet, it was only possible to have a laboratory diagnosis of the disease in MBCH. Thus, only about 10% of all patients who got malaria diagnosis and treatment had laboratory verified malaria. For prevention there was distribution of bed-nets, initially both through the public services as well as private channels. Later they were only to be given free of charge through government officials, considered by health professionals to hamper their distribution and use. Data indicate that the distribution was effective, compared to many other low-income countries as the coverage of bed-net use increased from 3% in 2001 to 66% in 2013 (United Nations 2015)
HIV/AIDS. In April 2005 a VCT-clinic (Volunteer Counseling Testing, now called HCT (HIV Counseling and Testing)) was installed in MBCH to serve HIV infected patients, their families, as well as for pregnant women. It was the first one in Mangochi District outside the District Hospital (MDH), and was placed in one small room in the administration building (Gunnlaugsson 2007). In December 2005, another HCT was established in Nankumba health facility. In June 2006 further improvement occurred when ARV (anti-retroviral) treatment unit was established in the MBCH. HIV-positive patients who fulfilled certain clinical criteria, as defined by the World Health Organization, received medical treatment to hamper progress of the disease. In light of the great demand, a new facility was constructed for this service, taken into use in October 2007.
Data from the services give a clear indication of their necessity. In the period 2005 to 2014, in total 53.635 patients were seen in VCT/HCT, on average 5.977 patients per year (median 6.807, range 2.389-10.924). In MBCH, 22.100 patients were attended in the period or 42% of the total, and health professionals in government run facilities (MBCH and Nankumba) attended 58% of all attendees.
A study conducted in 2007 concluded that 1.257 (25%) were HIV positive out of 5043 patients who had attended the clinic since its establishment (Arnardóttir 2007). About half of those who attended were pregnant women and 15% of them HIV positive. In addition, in less than one year (June 2006 to March 2007), 317 patients had initiated ART for their symptoms of AIDS, and 111 newborns were given ART for preventive purposes.
A qualitative study was conducted on the VCT in the area to explore young women’s vulnerability towards HIV infections thought to arise from harmful gender norms and cultural practices (Pétursdóttir 2010). Nurses interviewed and involved in the VCT clinic emphasized that it was not compulsory for pregnant women to attend the clinic but highly recommended. After initial hesitation, the women got used to it and attended freely in all the health facilities. This was facilitated by the fact that the test was a prerequisite for access to ‘Prevention of Mother-to-Child Transmission’ (PMTCT) services to limit the spread of the disease to their newborns. In addition to the VCT clinic in MBCH, an out-reach VCT clinic operated weekly in Nankumba and Malembo since December 2005. Further, it was concluded that social relations of women are more complicated than prevailing ideas of women as defenseless victims with little or no agency vis-à-vis HIV/AIDS.
Outcome indicators
There are no solid outcome data available from the Monkey Bay area, but they are costly and difficult to obtain. Yet, at the start of project activities in 2000 in the Monkey Bay area, the IMR in Malawi was estimated to be 135 and U5MR 234 per 1000 live births. In 2011, these rates were estimated to be 69 and 110, respectively, a significant decline.
Maternal mortality rates (MMR) are notoriously more difficult to evaluate. In the year 2000, MMR was estimated to be 620 per 100.0000 live births, in 2009 about 1100, and in 2013 estimated to be 510 (Requejo, Victora, and Bryce 2015). This fluctuation reflects the difficulties to have good data on MMR.
Results from the baseline study in 2009 can also serve as indicators to measure outcome (Gunnlaugsson and Einarsdóttir 2009). In contrast to the situation in 1999, in 2009 MBCH was considered as a good hospital that had lifted the burden of people of traveling to Mangochi for health care. For the population, distance is important for access and ambulance services were well received. Some argued that MBCH worked almost like a district hospital and was in some aspects even a better hospital than MDH. Health centre staff in all the facilities, government run as well as CHAM, were also pleased with the hospital and argued that it helped with transport vehicles, supervision and technical assistance in the care of patients. Attention was called to overcrowding at the OPD in MBCH with long waiting times, a complaint reacted upon in 2011 with new and expanded OPD and waiting area. In all the corners of the Monkey Bay health area visited, it was claimed that MBCH served the communities, “they all come to Monkey Bay when seriously sick.” For all the health centres in the zone, MBCH served as a first point of referral for complicated cases. Before its establishment with Iceida’s support everybody was referred directly to MDH, now everybody preferred MBCH (Gunnlaugsson and Einarsdóttir 2009).
Discussion
Here we present data from the implementation of the MBHCP by Iceida in the Monkey Bay area in southern Malawi in the period 2000-2011. It is the largest development project the Agency has undertaken within the health sector. The evaluation of project activities presented is based on several monitoring and evaluation principles, specific research work of university students and the authors, and regular consultative work by one of the authors (GG). It can be concluded on the basis of the data presented that the collaboration of Iceida with the GoM has strengthened and improved the healthcare services in the Monkey Bay area. Numerous internationally recognized indicators on structure and process of healthcare services indicate overall improvement of the services. In addition, qualitative data indicate acceptance and positive views of the population on the progress in service provision in the area. This is further strengthened with data that show increased attendance to services provided that expanded both in scope and content during the same period.
In general terms, health services aim to contribute to improved life and wellbeing of the population, and later socio-economic development. Such effects take however a long time to develop. Outcome indicators (Donabedian 1988) are the most important ones, for example infant (IMR) and U5-mortality rates (U5MR). These are however costly and difficult indicators to regularly monitor for an area of the size of Monkey Bay, and within a project as that of Iceida’s. Malawi is however one of few countries in sub-Saharan Africa that achieved MDG4 already in 2013, i.e., the one regarding IMR and U5MR (Kanyuka et al. 2016). Actually, the decline in U5MR in Malawi and some other low-income countries has been taken as a proof that low income need not be an impediment to saving children’s lives (United Nations 2015). On the other hand, Mangochi District is among those districts with least progress (U5MR decreased from 161 to 107 per 1000 live births) (Requejo, Victora, and Bryce 2015), an indication of the difficulties encountered in this setting and inter-district variability. This general positive outcome in Malawi vis-à-vis MDG4 would not have been possible without international support. The success of Malawi is claimed to be a result of a scale-up of interventions such as programmes to improve treatment of major childhood diseases associated with high mortality (malaria, pneumonia and diarrhoea), programmes to reduce mother-to-child transmission of HIV, and improvement in the quality of care provided to women around birth and their newborn (Kanyuka et al. 2016). These are interventions that Iceida supported along the years of project implementation in the Monkey Bay health area, as described above.
All along project implementation in the Monkey Bay health area there were continuous efforts to monitor and improve the quality of the HMIS (Gunnlaugsson 2011). Within the system there are numerous process indicators (Donabedian 1988) that can be monitored month-by-month and year-by-year. Such data include for example data on attendance to services (OPD, ANC, skilled birth attendance, vaccination, outreach, admittance to wards, HCV clinic and ART, etc), and these show general improvement and attraction of governmental services to the population, as presented above. Qualitative improvement in the services can also be seen in the sheer number and variety of surgical interventions in MBCH, an activity introduced in the area with Iceida’s support. Process data also indicate improved access to ART in the area, which is a qualitative improvement similar to the one experienced in Karanga District in northern Malawi. There, four years after the introduction of ART, all-cause mortality of adults showed dramatic decline with no evidence of an increase in deaths due to non-communicable diseases (Chihana et al. 2012). Yet, such services and preventive efforts could be far more effective should attention be given to women’s lived realities and on-the-ground interpretations of women’s agency (Pétursdóttir 2010).
Structural indicators are the easiest to monitor and register (Donabedian 1988). These may not be as relevant in high-resource settings while they are crucial indicators to monitor the development of health services in low-income countries, as those in sub-Saharan Africa. Numerous structural indicators point to the success of Iceida’s project in this respect. Improved and expanded physical structures are evidenced in new and renovated government run facility buildings, staff houses, and transport vehicles, including ambulant services.
Despite continuous efforts to improve the HMIS within the Monkey Bay health area, there is still need to train staff in its use and application, exemplified by incomplete data from the area for the period 2012-2014, that is, after termination of project activities. This experience is however not restricted to Monkey Bay or Malawi (Gerrets 2015), and will need continued support and engagement. Nevertheless, despite data not being complete, as is also the case of data on outreach services (Jónsdóttir 2006), available data give a good indication on the importance and acceptance of such service by the population, and is a good indicator on how deeply the services reach into distant rural communities. Further, data on the community health services, with high number of TBAs and CBDAs receiving training and access to relevant materials give a clear indication on widely project activities reached to the poor in the area.
The question of sustainability is always of concern for development project implementation. All through the collaboration in the Monkey Bay area in 1999-2011 it was common knowledge that the GoM would have no means to cover by itself all the costs associated with health service delivery, neither in Monkey Bay nor elsewhere in the country (Kanyuka et al. 2016). Thus, outside assistance will be necessary for years to come, e.g., through budget support or project support such as that of Iceida. Despite difficulties shared with many low-income countries, all through the implementation of project activities in Monkey Bay the Malawian authorities were keen to stand up to the challenge to fulfill their contractual obligations.
In total, Iceida contributed $7.5m or about $4 per capita and year to the health services in the Monkey Bay health area. It is estimated that $44 per person and year are needed to provide basic, life-saving services (World Health Organization 2012), including settings as the one found in Monkey Bay. These data are a sober reminder of the precarious financial situation many poor countries face vis-à-vis the aim to fulfill the aspirations of their populations for good quality health services. Based on the experience achieved in Monkey Bay area, at termination of project activities, Iceida embarked in 2012 on ambitious district wide development assistance to improve basic services in all of Mangochi District, including public health, education and water-and-sanitation (Iceida 2012), and the collaboration is expected to be extended after 2016.
The expected output of project activities for MBCH to become a fully fledged community hospital was not achieved. To become one it lacked at project termination special paediatric and isolation wards, kitchen, X-ray department and a Nutritional Rehabilitation Unit. After the termination of Iceida’s support, the Malawian authorities installed an X-ray department, one example of their commitment to have a fully fledged community hospital in the area. In addition, documented data in the health information system, the baseline study conducted in 2009, student research assignments, case histories as well as numerous accounts of people who prefer to go to MBCH rather than to MDH are evidence of that MBCH has become the first choice for health care services in the area. However, it can also be assumed that activities within water-and-sanitation, adult literacy program, small-scale fishery technology program and construction of primary schools in the area have without doubt further increased visibility of Iceida’s work in the area, and its appreciation (Iceida n.d.).
The issue of user-charges has been highly debated within global health. After a long period of claims of the importance of applying user-fees for sustainable health services, universal health coverage (UHC) is now agreed to be an important element for successful outcome of the SDG3 (WHO, 2015). Data presented here from the Monkey Bay health area indicate how user-fees may change care-seeking behaviour. Despite expressed critic against user-fees applied in the NGO run CHAM services in the area (Gunnlaugsson and Einarsdóttir 2009) parents tend to attend with their children to such facilities while adults attend government run facilities that do not apply user charges. This discrepancy may indicate that adults take the view that they tolerate sickness better than children, and can seek care for themselves that is free of charge, despite longer distances, while they bring their children to the nearest health facility, despite its associated costs. Yet, as international development agencies are known for herding behaviour regarding policy and implementation (Einarsdóttir and Gunnlaugsson 2005; Einarsdóttir and Gunnlaugsson 2016) it is to be hoped that the goal of UHC will materialize to the benefit of the poor in sub-Saharan Africa.
Conclusions
Lessons learned from Iceida’s support to the health care system in Monkey Bay area during the period 2000-2011 are several. First, the contracting parties for project implementation succeeded to foster good relations and mutual understanding regarding the project activities. Second, Malawian health authorities, both at the level of the Ministry and Mangochi District Health Management Team supported the project activities, e.g. evidenced through increasing number of staff in MBCH, and other input to improve the services. Third, project activities within the health sector reached deep into involved communities and gave much needed health service for the rural poor. Through its activities, ICEIDA gave the GoM support in its strive to reach the MDG4-6 and contributed to strengthen international collaboration in line with MDG8. Four, project efforts by a small organization such as ICEIDA in a well-defined area, such as Monkey Bay, has the potential to transform governmental services to the benefit of those it is intended to serve, the rural poor. The experience gained is the foundation on which the current expanded support of Iceida to public health, education and water-and-sanitation in Mangochi District is built. Five, alignment of project activities within the framework of national health policy and priorities contributed to the success of Iceida’s investment in the area, as described here. Finally, while sustainability of project activities was the over-all aim of Iceida’s support, in the foreseeable future Malawi has no possibility to fund health services without external support, be it through project support as in the case of MBHCP, or budget support by other international donors.
Following the devastating Ebola epidemic in West Africa, the call for health system strengthening in the spirit of Alma Ata has once again become urgent, ‘now more than ever’ (World Health Organization 2008; Moon et al. 2015). The Ebola epidemic and fragile health systems in the affected areas are a sober reminder of the importance of work as the one Iceida has been engaged in the Monkey Bay area since 2000, and now in all Mangochi District. It may not exclude the possibility of difficult epidemics, but strengthened health system will be in better shape to successfully tackle such challenges.
References
Arnardóttir, Lilja Rut. 2007. “Diagnosis and Treatment of HIV/AIDS in Monkey Bay Community Hospital.” Reykjavík: Faculty of Medicine, University of Iceland and the Icelandic International Development Agency (Iceida).
Bamberger, Michael. 2012. “Introduction to Mixed Methods in Impact Evaluation.” Impact Evaluation Notes 3: 1–38.
Bamberger, Michael, Jim Rugh, Mary Church, and Lucia Fort. 2004. “Shoestring Evaluation: Designing Impact Evaluations under Budget, Time and Data Constraints.” American Journal of Evaluation 25 (1): 5–37. doi:10.1177/109821400402500102.
Bennett, S., T. Woods, W. M. Liyanage, and D. L. Smith. 1991. “A Simplified General Method for Cluster-Sample Surveys of Health in Developing Countries.” World Health Statistics Quarterly. Rapport Trimestriel De Statistiques Sanitaires Mondiales 44 (3): 98–106.
Better Evaluation. 2015. “Equal Access Participatory Monitoring and Evaluation Toolkit | Better Evaluation.” Accessed October 29, 2015. http://betterevaluation.org/toolkits/equal_access_participatory_monitoring.
Chihana, Menard, Sian Floyd, Anna Molesworth, Amelia C Crampin, Ndoliwe Kayuni, Alison Price, Basia Zaba, et al. 2012. “Adult Mortality and Probable Cause of Death in Rural Northern Malawi in the Era of HIV Treatment.” Tropical Medicine & International Health 17 (8): e74–83. doi:10.1111/j.1365-3156.2012.02929.x.
Conlin, Sean, and Roderick L. Stirrat. 2008. “Current Challenges in Development Evaluation.” Evaluation 14 (2): 193–208. doi:10.1177/1356389007087539.
Davis, Kevin E., Benedict Kingsbury, and Sally Engle Merry. 2010. “Indicators as a Technology of Global Governance.” SSRN Scholarly Paper NYU Law and Economics Research Paper No. 10-13; NYU School of Law, Public Law Research Paper No. 10-26. Rochester, NY: Social Science Research Network. http://papers.ssrn.com/sol3/papers.cfm?abstract_id=1583431.
Donabedian, A. 1988. “The Quality of Care: How Can It Be Assessed?” JAMA 260 (12): 1743–1748. doi:10.1001/jama.1988.03410120089033.
Einarsdóttir, Jónína, and Geir Gunnlaugsson. 2005. “International Aid, Partnership, and Child Survival.” The Lancet 365 (9465): 1135–1136.
———. 2016. “Applied Ethics and Allocation of Foreign Aid: Disparity in Pretensions and Practice.” Development Policy Review 34 (3): 345–363.
Fjalldal, Sigríður Bára. 2004. “Antenatal Care Services in Monkey Bay Head Zone, Malawi.” Reykjavik: Faculty of Medicine, University of Iceland and the Icelandic International Development Agency (Iceida).
Gerrets, René. 2015. “Charting the Road to Eradication: Health Facility Data and Malaria Indicator Generation in Rural Tanzania.” In The World of Indicators: The Making of Governmental Knowledge through Quantification (Cambridge Studies in Law and Society, edited by R Rottenburg, S.E. Merry, S.J. Park, and J Mugler, 151–87. Cambridge: Cambridge University Press.
Gillam, Stephen. 2008. “Is the Declaration of Alma Ata Still Relevant to Primary Health Care?” BMJ : British Medical Journal 336 (7643): 536–538. doi:10.1136/bmj.39469.432118.AD.
Guðmundsdóttir, Berglind Eik. 2006. “Care of Sick Neonates at Monkey Bay Community Hospital in Malawi.” Reykjavík: Faculty of Medicine, University of Iceland and the Icelandic International Development Agency (Iceida).
Gunnlaugsson, Geir. 2007. “Alnæmi í Afríku Sunnan Sahara [e. HIV/AIDS in Sub-Saharan Africa].” Þróunarmál. Fréttabréf Þróunarsamvinnustofnunar [e. Development Issues – Iceida’s Newsletter] 21(1):11-15.
———. 2011. “Monkey Bay Health Care Project: Final Report.” Reykjavík: Icelandic International Development Agency (Iceida) and the Directorate of Health.
Gunnlaugsson, Geir, and Jonina Einarsdóttir. 2009. “Baseline Study on the Health Care Services in the Monkey Bay Area, Mangochi District, Malawi.” Reykjavik: Reykjavík University and the Icelandic International Development Agency. http://www.iceida.is/media/pdf/Report_November_3,_2009.pdf.
Iceida. n.d. “Evaluation Reports and Reviews.” Icelandic International Development Agency. http://www.iceida.is/utgefid-efni/uttektir/uttektaskyrslur/#
Iceida. 2012. Mangochi Basic Services Programme. Master Programme Document. Reykjavík, Lilongwe, and Mangochi: Iceida, Ministry of Local Government and Rural Development (MoLGRD), and Mangochi District Council. http://bit.ly/1SJLb2Q
ICSU, and ISSC. 2015. “Review of Targets for the Sustainable Development Goals: The Science Perspective.” Paris: International Council for Science (ICSU). http://bit.ly/24hmuN2
Jónsdóttir, Björg. 2006. “Out-Reach Clinics in Monkey Bay, Malawi.” Reykjavík: Faculty of Medicine, University of Iceland and the Icelandic International Development Agency (Iceida).
Kanyuka, Mercy, Jameson Ndawala, Tiope Mleme, Lusungu Chisesa, Medson Makwemba, Agbessi Amouzou, Josephine Borghi, et al. 2016. “Malawi and Millennium Development Goal 4: A Countdown to 2015 Country Case Study.” The Lancet Global Health, Mar;4(3):e201-14 doi:10.1016/S2214-109X(15)00294-6.
Kriel, Antoinette, Sara Randall, Ernestina Coast, and B. de Clercq. 2014. “From Design to Practice: How Can Large-Scale Household Surveys Better Represent the Complexities of the Social Units under Investigation?” 28 (3): 1309–1323.
Kumar, Krishna. 1989. “Indicators for Measuring Changes in Income, Food Availability and Consumption, and the Natural Resource Base.” U.S. Agency for International Development.
Lawn, Joy E, Jon Rohde, Susan Rifkin, Miriam Were, Vinod K Paul, and Mickey Chopra. 2008. “Alma-Ata 30 Years on: Revolutionary, Relevant, and Time to Revitalise.” The Lancet 372 (9642): 917–27. doi:10.1016/S0140-6736(08)61402-6.
MDF Training and Consultancies. 2005. “Indicators.” MDF. http://bit.ly/1rwHC4g
Ministry of Health. 2009. “Health Information Systems Health Information Systems. Assessment Report 2009.” Lilongwe, Malawi: Ministry of Health and Health Metrix Network. http://www.who.int/healthmetrics/library/countries/2HMN_MWI_Assess_Final_2009_07_en.pdf.
Moon, Suerie, Devi Sridhar, Muhammad A Pate, Ashish K Jha, Chelsea Clinton, Sophie Delaunay, Valnora Edwin, et al. 2015. “Will Ebola Change the Game? Ten Essential Reforms before the next Pandemic. The Report of the Harvard-LSHTM Independent Panel on the Global Response to Ebola.” The Lancet 386 (10009): 2204–21. doi:10.1016/S0140-6736(15)00946-0.
OECD/DAC. 2010. “Glossary of Key Terms in Evaluation and Results Based Management.” OECD. http://www.oecd.org/dac/evaluation/2754804.pdf.
Pétursdóttir, Inga Dóra. 2010. “‘If I Had a Spear, I Would Kill the HIV Beast.’ Views from a Malawian Village on the HIV Epidemic.” Masters thesis (MA) in Development Studies, Reykjavík: Faculty of Social Sciences, University of Iceland. http://hdl.handle.net/1946/4875.
Ragnarsson, Sigurður, Lovísa Leifsdóttir, Fredrick Kapinga, and Geir Gunnlaugsson. 2006. “Heilbrigðisþjónusta við veik börn með IMCI vinnuferlum í Monkey Bay, Malaví [e. Health services for children and the implementation of IMCI in Monkey Bay, Malawi]” Laeknabladid 92:271-279. http://www.laeknabladid.is/2006/04/nr/2303.
Randall, Sara, Ernestina Coast, and Tiziana Leone. 2011. “Cultural Constructions of the Concept of Household in Sample Surveys.” Population Studies 65 (2): 217–229. doi:10.1080/00324728.2011.576768.
Requejo, Jennifer, Cesar Victora, and Jennifer Bryce. 2015. “A Decade of Tracking Progress for Maternal, Newborn and Child Survival. The 2015 Report.” Draft. New York: Unicef and World Health Organization. http://bit.ly/1VPR6nV
Salimu, Thomas Claydon. 2004. “Assessing the Functioning of the Health Management Information System (HMIS) at Monkey Bay Rural Community Hospital.” Blantyre: College of Medicine, University of Malawi.
Segone, Marco. 2008. “Bridging the Gap. The Role of Monitoring and Evaluation in Evidence-Based Policy Making.” UNICEF, World Bank and the International Development Evaluation Association. http://www.unicef.org/ceecis/evidence_based_policy_making.pdf.
Snæbjörnsson, Thorkell. 2007. “Malaria and Its Prevention in Monkey Bay, Malawi.” Reykjavík: Faculty of Medicine, University of Iceland.
Stefánsdóttir, Eva Laufey. 2006. “The Role of Traditional Birth Attendants in Monkey Bay Area, Malawi.” Final assignment for a degree in midwifery. Reykjavík: Faculty of Nursing, University of Iceland.
Sustainable Development Knowledge Platform. 2015. “Sustainable Development Goals.” September. https://sustainabledevelopment.un.org/?menu=1300.
The DHS Program. 2015. “The DHS Program – Quality Information to Plan, Monitor and Improve Population, Health, and Nutrition Programs.” Accessed October 28. http://dhsprogram.com/.
Thórdarson, Thórdur Thórarinn, Ásgeir Haraldsson, Halldór Jónsson, Richard G. Chola, and Geir Gunnlaugsson. 2005. Þekjun bólusetningar barna við Monkey Bay, Malaví [e. Coverage of immunisation of children in Monkey Bay, Malawi]. Læknabladid 91:649-654. http://www.laeknabladid.is/2005/09/nr/2089
Unicef. 2015. “UNICEF MICS.” Accessed October 28. http://mics.unicef.org/.
United Nations. 2015. “The Millennium Development Goals Report 2015.” New York: United Nations. http://bit.ly/1qPanYZ.
UN Millennium Project. 2000a. “Millennium Development Goals.” September. http://www.unmillenniumproject.org/goals/.
———. 2000b. “Millennium Development Goals.” September. http://www.unmillenniumproject.org/goals/.
WHO. 2015. “Health in 2015: From MDGs to SDGs.” WHO. Accessed December 11. http://www.who.int/gho/publications/mdgs-sdgs/en/.
World Health Organization. 1978. “Declaration of Alma-Ata, 1978.” http://www.who.int/publications/almaata_declaration_en.pdf.
———. 2008. “The World Health Report 2008. Primary Health Care Now More Than Ever.” Geneva: World Health Organization. http://www.who.int/whr/2008/en/.
———. 2012. “Spending on Health: A Global Overview. Fact Sheet N°319.” World Health Organization. http://www.who.int/mediacentre/factsheets/fs319/en/.